Muscle Memory: How Our Bodies Store Trauma
If you struggle with anxiety, we recommend trying out Rewire Your Anxious Brain by clicking HERE to get it from Amazon for only $13.
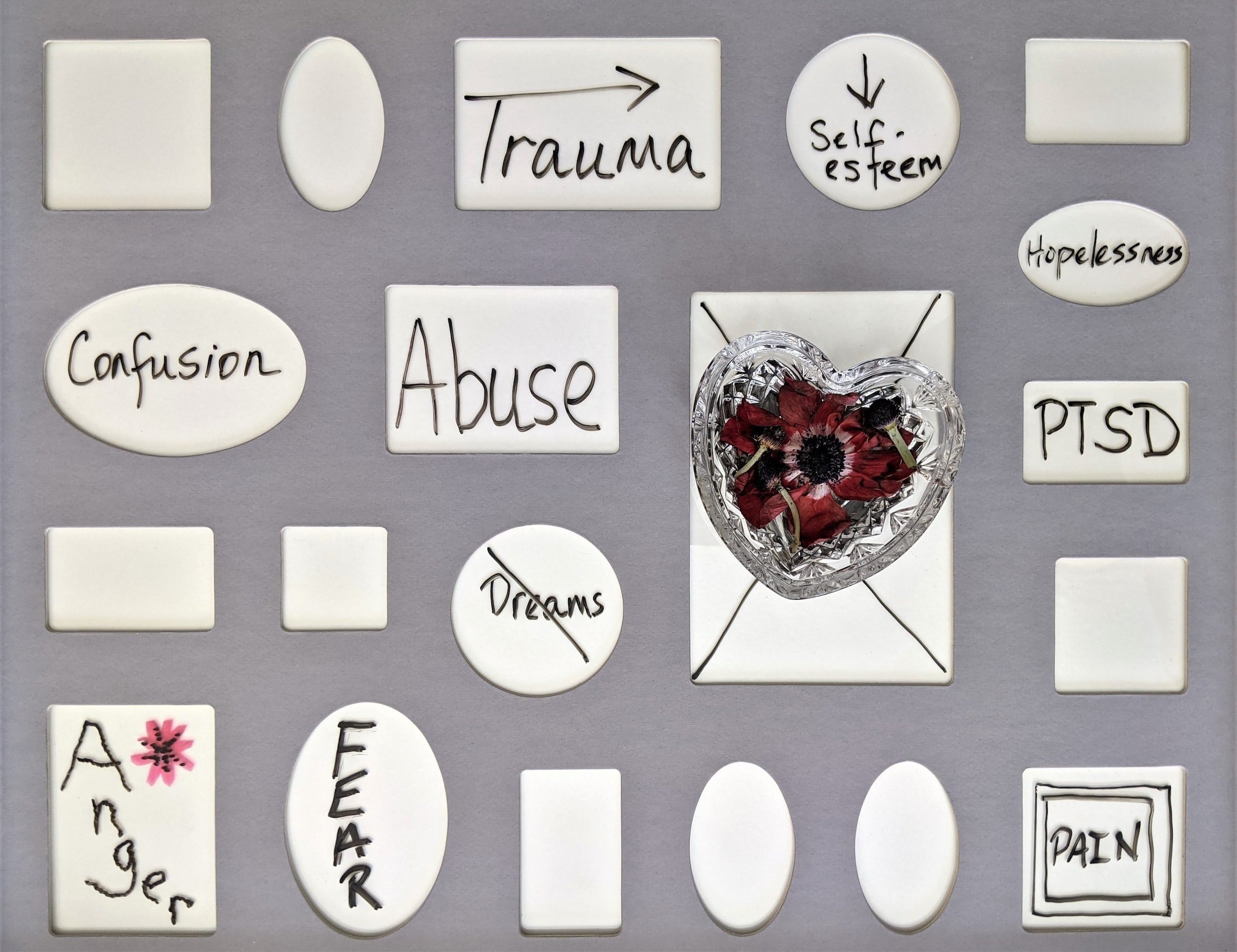
Trauma is an experience that can have long-lasting effects on an individual's mental and physical well-being. While traditional talk therapies can be helpful in addressing the psychological impacts of trauma, it's also important to acknowledge how trauma lives in the body.
What is Trauma?
Trauma can be defined as a "distressing or life-threatening experience that overwhelms an individual's ability to cope" (van der Kolk, 2014). During a traumatic experience, the body activates the fight-or-flight response, which involves the release of stress hormones such as cortisol and adrenaline. This response can help individuals survive in the short term, but if the traumatic experience is ongoing, the body can become stuck in a state of hyperarousal.
How Does Trauma Develop in the Body?
One of the ways trauma can live in the body is through the development of chronic pain. Studies have shown that individuals who have experienced trauma are more likely to develop chronic pain conditions such as fibromyalgia, back pain, and headaches (Afari et al., 2014). This may be due to the fact that trauma can alter the way the nervous system processes pain signals, leading to increased sensitivity and a lower pain threshold.
Trauma can also affect the immune system, leading to a heightened inflammatory response. Chronic inflammation has been linked to various health conditions, including heart disease, diabetes, and autoimmune disorders (Miller et al., 2011). This suggests that trauma can have long-term effects on physical health, even years after the initial traumatic experience.
Furthermore, trauma can manifest in the body through somatic symptoms such as nausea, dizziness, and difficulty breathing. These symptoms may not have a clear physical cause and can be difficult to treat with traditional medical interventions. It's important to acknowledge how trauma lives in the body, as this can inform the development of holistic treatment approaches that address both the psychological and physical impacts of trauma. Body-based therapies such as yoga, massage, and acupuncture have been found to be effective in reducing somatic symptoms related to trauma (Price et al., 2017).
Evicting Trauma from the Body
There is a range of therapeutic techniques that can be effective for addressing trauma in the body, including somatic experiencing, EMDR (eye movement desensitization and reprocessing), and mindfulness-based interventions (Price et al., 2018). By integrating body-based therapies into traditional talk therapy, individuals can work towards healing their minds and bodies. These approaches can help individuals to reconnect with their bodies, release physical tension and emotional blockages, and develop new ways of relating to their experiences.
Trauma can take many forms and can have a profound impact on the human body. From physical injuries to emotional wounds, trauma can cause many physical and psychological symptoms affecting a person's overall well-being (Kira et al., 2012). In this article, we will explore the different kinds of trauma and their effects on the body.
Physical trauma is any injury to the body that is caused by an external force. This can include anything from a broken bone to a gunshot wound. Physical trauma can immediately affect the body with symptoms, such as pain, swelling, and bruising. However, the long-term effects of physical trauma can be just as significant. Chronic pain, limited mobility, and a higher risk of developing chronic health conditions are all potential consequences of physical trauma (CDC, 2022).
Emotional trauma is a type of trauma that affects a person's psychological well-being. Emotional trauma can be caused by various experiences, including abuse, neglect, and witnessing or experiencing a traumatic event. The effects of emotional trauma can be long-lasting and may manifest as anxiety, depression, and post-traumatic stress disorder (PTSD) (Briere & Scott, 2015). Additionally, emotional trauma can physically affect the body, such as headaches, digestive issues, and chronic pain (Walker et al., 2013).
Sexual trauma is a form of emotional trauma caused by sexual assault or abuse. The effects of sexual trauma can be severe and long-lasting and can include symptoms such as anxiety, depression, and PTSD. Sexual trauma can also physically affect the body, such as chronic pain, digestive issues, and sexual dysfunction (Tolin & Foa, 2006).
Childhood trauma is any trauma that occurs during a person's formative years, typically before the age of 18. Childhood trauma can take many forms, including physical abuse, emotional abuse, neglect, and sexual abuse. The effects of childhood trauma can be long-lasting and may manifest as anxiety, depression, and PTSD. Additionally, childhood trauma can affect a person's physical health, leading to chronic health conditions such as heart disease, obesity, and diabetes (Felitti et al., 1998).
Click HERE for a fantastic resource on facing life’s toughest challenges and regaining control of your body’s trauma response.
Racial trauma is a form of emotional trauma caused by experiencing or witnessing racism and discrimination. It can include direct experiences of racism, such as being the target of racial slurs or hate crimes, and indirect experiences, such as watching videos of police brutality against people of color. Racial trauma can have profound psychological effects, such as anxiety, depression, and PTSD. Additionally, racial trauma can physically affect the body, such as headaches, digestive issues, and chronic pain (Carter et al., 2020).
Combat trauma, also known as military trauma, is a form of emotional trauma that is experienced by military personnel who have been exposed to combat. The effects of combat trauma can be severe and long-lasting and include symptoms such as anxiety, depression, and PTSD. Additionally, combat trauma can physically affect the body, such as chronic pain, hearing loss, and traumatic brain injury (TBI) (Vasterling et al., 2012).
Conclusion
These are just a few examples of the many types of trauma that people can experience throughout their lives. Whether trauma comes from a single event or ongoing stressors, it can affect our bodies, minds, and emotions. Recognizing and addressing trauma in the body is an important step toward healing and recovery. With the help of a trained therapist or other healthcare providers, it is possible to work through trauma and find new ways of relating to our experiences. Trauma is a complex and multifaceted experience that can have profound and lasting effects on our physical, emotional, and mental health. By understanding how trauma lives in the body and learning to recognize and address its symptoms, we can begin to heal and move forward with our lives. If you or someone you love are struggling with the after-effects of trauma, know that you are not alone and that help is available.
Resources
These resources provide services and support for individuals who have experienced trauma, including counseling, support groups, crisis hotlines, and educational resources. It's important to remember that seeking help is a sign of strength, and these resources are available to provide support and guidance to those in need.
National Institute of Mental Health (NIMH)
Phone: 1-866-615-6464
Email: nimhinfo@nih.gov
National Child Traumatic Stress Network (NCTSN)
Phone: 1-310-235-2633
Email: info@nctsn.org
Phone: 1-800-273-8255 (press 1)
Email: ncptsd@va.gov
Phone: 1-410-825-8888
Email: info@sidran.org
RAINN (Rape, Abuse & Incest National Network)
Phone: 1-800-656-HOPE (4673)
Online chat: https://hotline.rainn.org/online/terms-of-service.jsp
Phone: 1-866-488-7386
Text: Text START to 678678
American Psychological Association (APA)
Phone: 1-800-374-2721
Email: apa@apa.org
Substance Abuse and Mental Health Services Administration (SAMHSA)
Phone: 1-800-662-HELP (4357)
Online chat: https://www.samhsa.gov/find-help/national-helpline
Phone: 1-800-273-TALK (8255)
Email: info@mhanational.org
Text: Text HOME to 741741
References:
Afari, N., Ahumada, S. M., Wright, L. J., Mostoufi, S., Golnari, G., & Reis, V. (2014). Psychological trauma and functional somatic syndromes: A systematic review and meta-analysis. Psychosomatic Medicine, 76(1), 2-11.
Briere, J., & Scott, C. (2015). Principles of trauma therapy: A guide to symptoms, evaluation, and treatment. Sage Publications.
Carter, R. T., Lau, M., Johnson, V., & Kirkinis, K. (2020). Racial trauma: Theory, research, and healing: Introduction to the special issue. American Psychologist, 75(1), 1–5.
Centers for Disease Control and Prevention. (2022). Physical trauma. Retrieved February 28, 2022, from https://www.cdc.gov/injury/wisqars/physical-trauma.html
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., ... Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine, 14(4), 245–258.
Kira, I. A., Lewandowski, L., Templin, T., Ramaswamy, V., Ozkan, B., & Mohanesh, J. (2012). Measuring cumulative trauma dose, types, and profiles using a development-based taxonomy of traumas. Traumatology, 18(1), 17–26.
Miller, G. E., Chen, E., & Parker, K. J. (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137(6), 959-997.
Tolin, D. F., & Foa, E. B. (2006). Sexual trauma. In S. M. Turner & E. B. Foa (Eds.), Psychiatric care of the medical patient (pp. 501–524). American Psychiatric Publishing.
Price, C. J., Hooven, C., & Gray, M. (2017). Development and feasibility of a trauma-sensitive yoga program: A pilot study. Traumatology, 23(2), 223-230.
van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Penguin Books.
Vasterling, J. J., Proctor, S. P., Friedman, M. J., Hoge, C. W., Heeren, T., King, L. A., & King, D. W. (2012). PTSD symptom increases in Iraq-deployed soldiers: Comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress, 25(1), 62–69.
Walker, E. A., Newman, E., Dobie, D. J., Ciechanowski, P., & Katon, W. (2013). Validation of the PTSD checklist in an HMO sample of women. General Hospital Psychiatry, 25(2), 153–159.